Integrated Diagnostics: the missing link in early and accurate diagnosis
Despite the progress in medical technology, many diagnostic processes remain fragmented – with data dispersed across multiple devices and systems. This slows down assessments, increases the risk of errors, and hinders collaboration. Integrated diagnostics addresses this challenge by connecting diagnostic tools, patient data, and decision-makers into a single, streamlined workflow. In this blog, we explore how this approach enhances efficiency and improves outcomes at every level of care.
What is Integrated Diagnostics?
Integrated diagnostics is a coordinated approach to patient assessment that brings together data from various diagnostic disciplines to support faster, more accurate clinical decisions. By consolidating health information in a single, accessible digital location, it enables healthcare professionals to collaborate more effectively and develop personalized care plans [1].
Real integration requires more than data storage. It depends on robust IT infrastructure, standardized data formats for system interoperability, and the widespread adoption of electronic health records (EHRs). True integration also means using diagnostic devices that automatically transfer data to the EHR – eliminating manual steps that can introduce delays or errors [2].
AI further enhances integrated diagnostics by accelerating data analysis and uncovering patterns that might otherwise be missed [3]. While many of these technologies have existed for decades, cost and complexity kept them fragmented. Today, advancements in hardware, connectivity, and software have made integrated diagnostics a practical and scalable reality [4].
What are the benefits of Integrated Diagnostics?
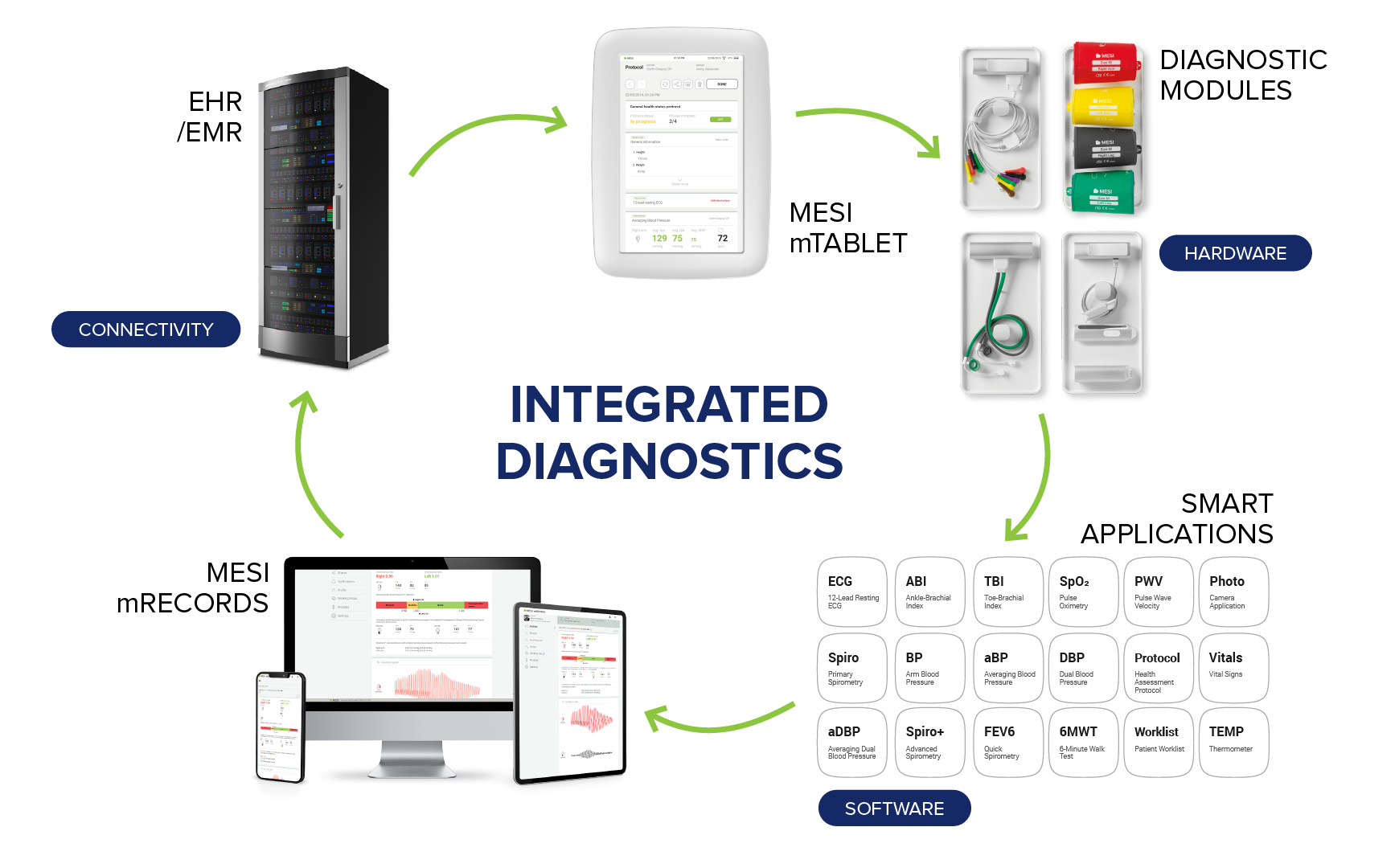
MESI's Integrated Diagnostics

Easier access to reliable health data
Integrated diagnostics builds on the foundation of EHRs, providing a centralised and standardised digital environment for patient data. One of the most significant benefits is improved data reliability – a critical factor in reducing medical errors. In the United States alone, such errors are estimated to be the third leading cause of death, contributing to over 250,000 fatalities annually [5].
These errors often stem from preventable issues such as illegible handwriting or unclear documentation – long-standing concerns in medical practice that can lead to incorrect prescriptions and other serious consequences [6][7][8]. By digitising and standardising data entry, integrated diagnostics helps eliminate these risks.
The advantages extend beyond clinical accuracy. A study comparing malpractice claims found that only 6.1% of EHR users had a history of paid claims, compared to 10.8% of clinicians using paper records [9]. The reduction in legal risk underscores the impact of structured digital workflows on overall care quality.
Moreover, integrated diagnostics enhances efficiency by streamlining processes and improving access to patient information. This accessibility supports timely collaboration between healthcare professionals – a prerequisite for delivering coordinated, high-quality care [10][11].
Facilitating collaboration in healthcare
Effective collaboration – especially across disciplines – delivers clear benefits for patients and healthcare providers alike. Studies consistently show that collaborative care reduces morbidity and mortality, lowers the incidence of preventable adverse drug reactions, and leads to more accurate medication dosing [12][13][14]. This results in more effective treatment overall. For healthcare professionals, it also means less redundant work and greater job satisfaction [15].
Despite these advantages, many healthcare settings still struggle with barriers to collaboration. Hierarchical structures and role ambiguity are deeply rooted in organisational culture and difficult to change. However, other challenges, such as administrative burden and poor communication, can be significantly reduced using electronic health records (EHRs) [16]. EHRs improve information flow and ensure that everyone involved in a patient’s care has access to the same data, supporting better coordination and shared decision-making.
Collaboration is no longer optional – it is increasingly essential. The rising prevalence of multimorbidity demands an integrated and team-based approach to care [17]. This is particularly urgent in complex fields like oncology, where outcomes depend on timely, multidisciplinary input and seamless integration of diagnostic and therapeutic advances [18].
Streamlined workflows and reduced costs
Fragmented diagnostic and care pathways often lead to delays in treatment – with serious consequences for patients. When diagnostic tools and patient data systems don’t work together, critical time is lost. A nurse may use six different devices and three separate software platforms just to complete a basic assessment. Results must then be transcribed manually, increasing the risk of error and delaying decisions. This fragmentation directly contributes to missed or late diagnoses.
Beyond clinical benefits, integrated diagnostics also contributes to operational efficiency. By consolidating data and avoiding unnecessary repeat testing, it reduces waste and lowers treatment costs. While these financial gains may be most visible in private healthcare systems, the efficiency of integrated diagnostics can equally support investment in public healthcare – offering a strong case for broader adoption.
Improved patient outcomes
Integrated diagnostics is not only cost-effective – it also supports better patient outcomes. While data on patient experience is still emerging, early indications suggest that streamlined, coordinated care contributes to a more positive experience – by reducing delays, limiting unnecessary procedures, and improving communication across care teams [19].
As adoption of integrated diagnostic solutions grows, particularly across various levels of care, the evidence base for their clinical and experiential benefits will continue to expand. It helps reshape diagnostic pathways – with the goal of delivering faster, more accurate, and more patient-centred care.
How the MESI mTABLET simplifies diagnostic workflows
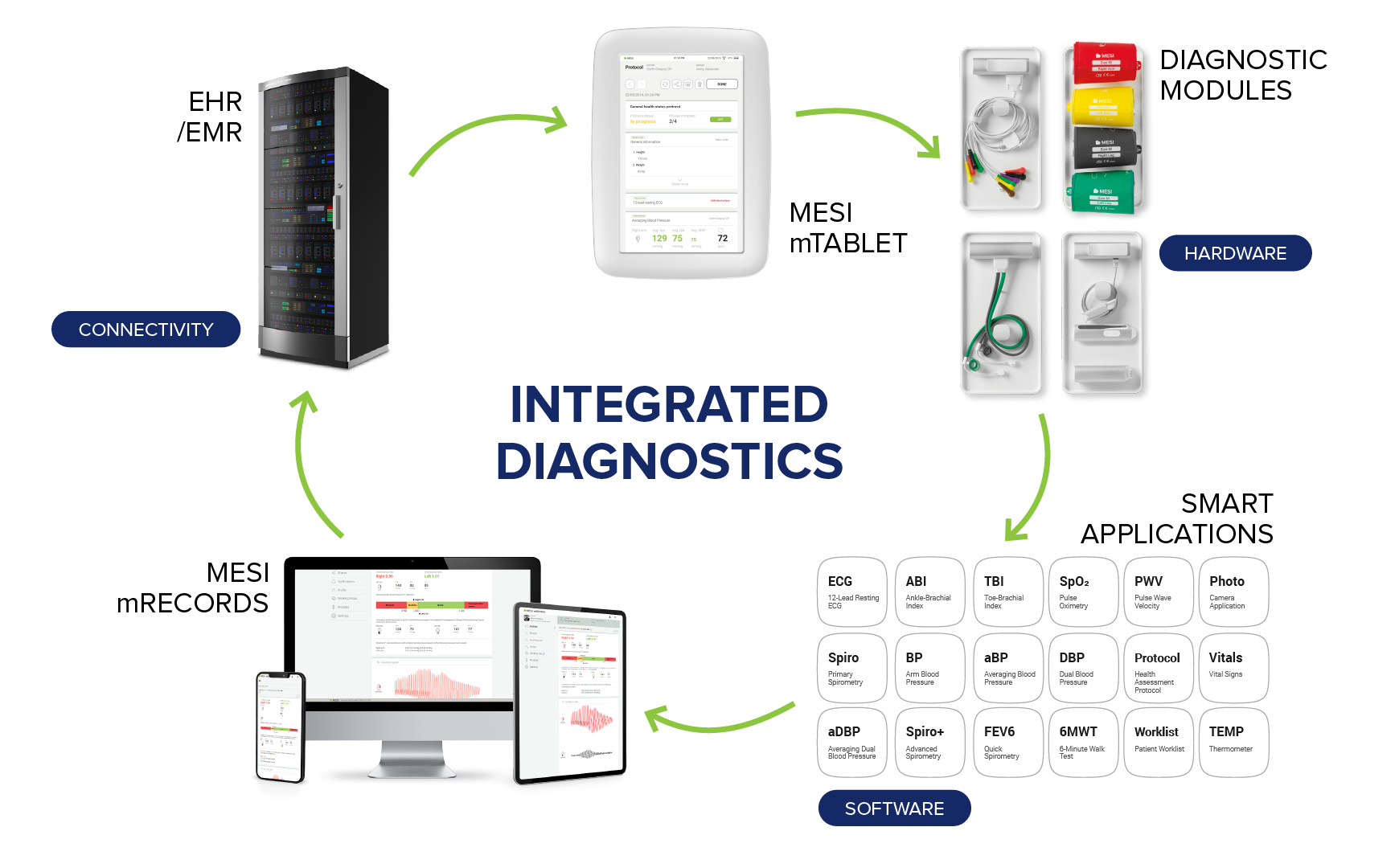
If integrated diagnostics is the engine of modern patient care, the MESI mTABLET is its driving force. Designed specifically for primary healthcare settings, it combines the functionality of a medical-grade tablet with wireless diagnostic modules and smart software to support efficient, data-driven decision-making. Its all-in-one approach eliminates the need for multiple devices and manual data entry, reducing administrative burden and the risk of errors – even in digital environments.
What sets the MESI mTABLET apart is its modularity. With a range of wireless diagnostic modules, it can perform:
The MESI mTABLET's integrated diagnostic approach simplifies workflows, enabling clinicians to spend less time managing equipment and more time with patients. This directly supports better experiences and outcomes, as shown by studies linking face-to-face time and streamlined care delivery to increased patient satisfaction and improved health results.