Automatische hilfsmittel in der Spirometrie
Die Spirometrie ist eine Diagnosemethode, bei der sich der Patient sehr anstrengen muss, damit der Test erfolgreich ist. Die digitale Technologie kann jedoch sowohl Ihnen als auch dem Patienten beim Untersuchungsprozess helfen. Die folgenden automatischen Funktionen des MESI mTABLET SPIRO können Ihnen helfen, den Patienten anzuleiten und die Qualität der Manöver auszuwerten, während und nachdem sie durchgeführt wurden.
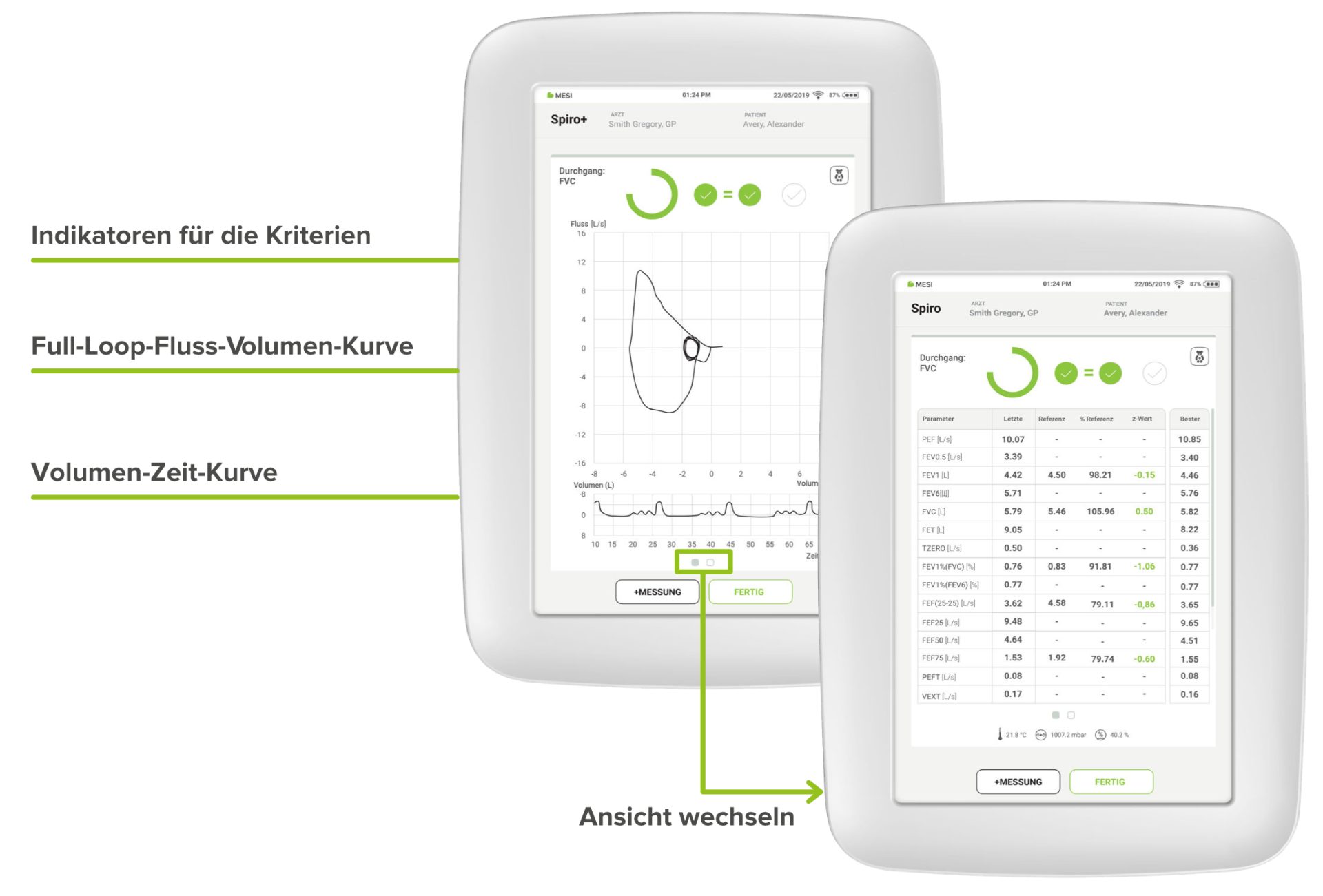
Echtzeitanzeige der Durchflussvolumenkurve
Während der Durchführung eines Manövers ist es möglich, das Manöver durch eine verbesserte visuelle Anzeige der Fluss-Volumen-Kurve und der Parameter zu überwachen. Sie können zwischen der Diagrammansicht und der Ansicht der Parameterwerte hin- und herwischen.
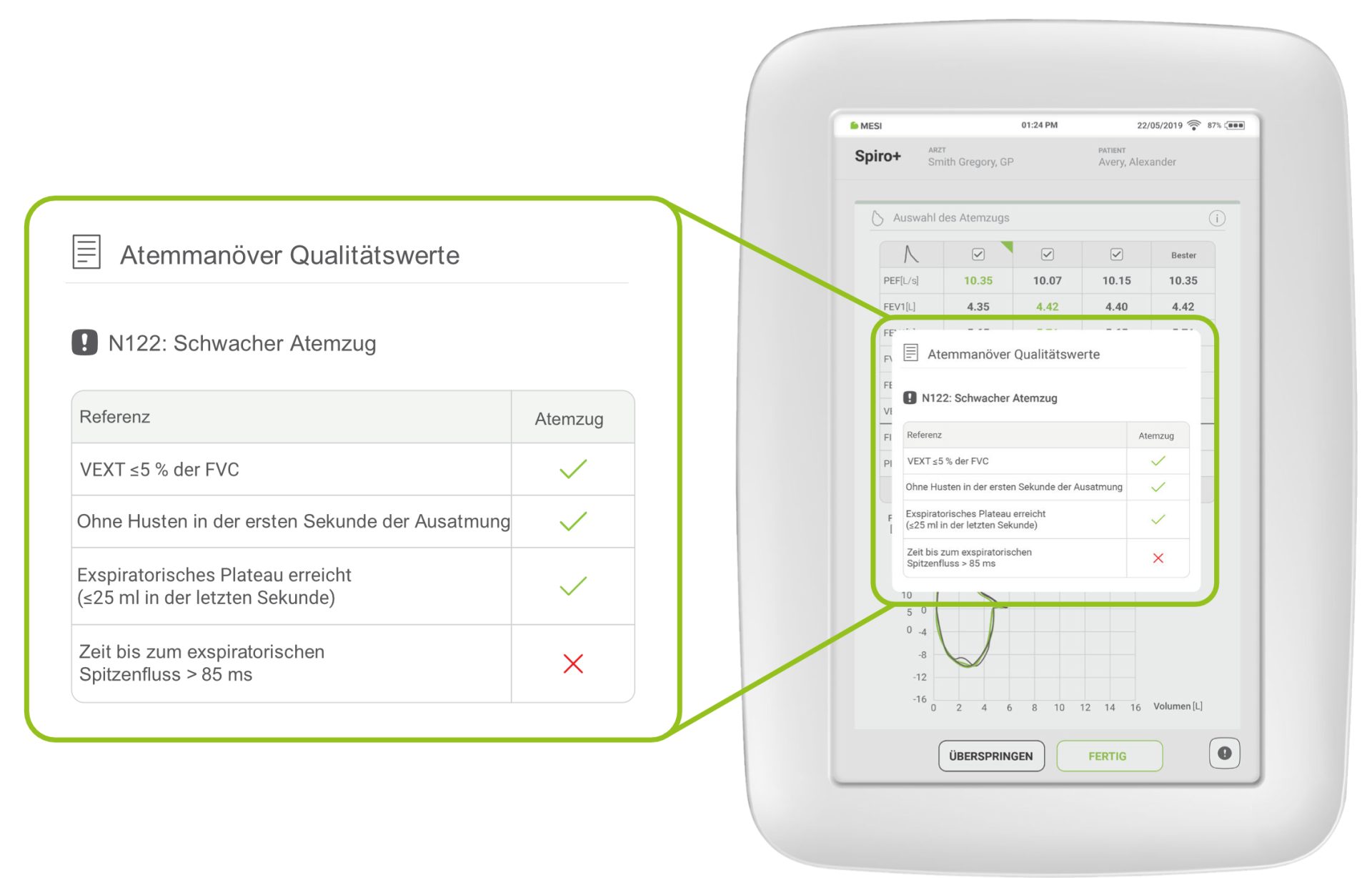
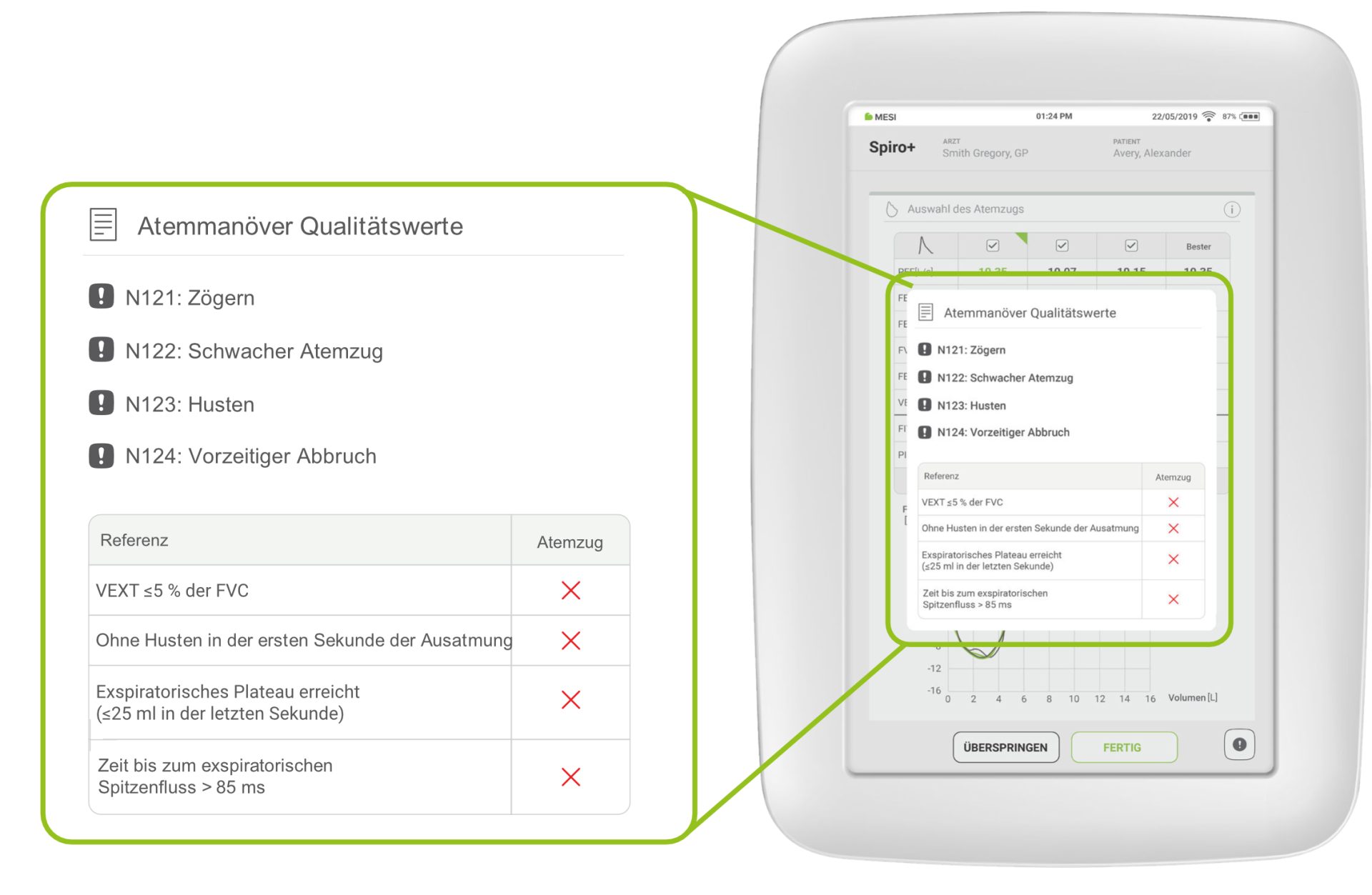
Warnhinweise zur Manöverqualität
Wenn das Gerät keine Qualitätsprobleme bei dem durchgeführten Manöver feststellt, erscheint ein grünes Häkchen. Im gegenteiligen Fall wird eine der folgenden Warnungen zur Manöverqualität auf dem Messbildschirm angezeigt:
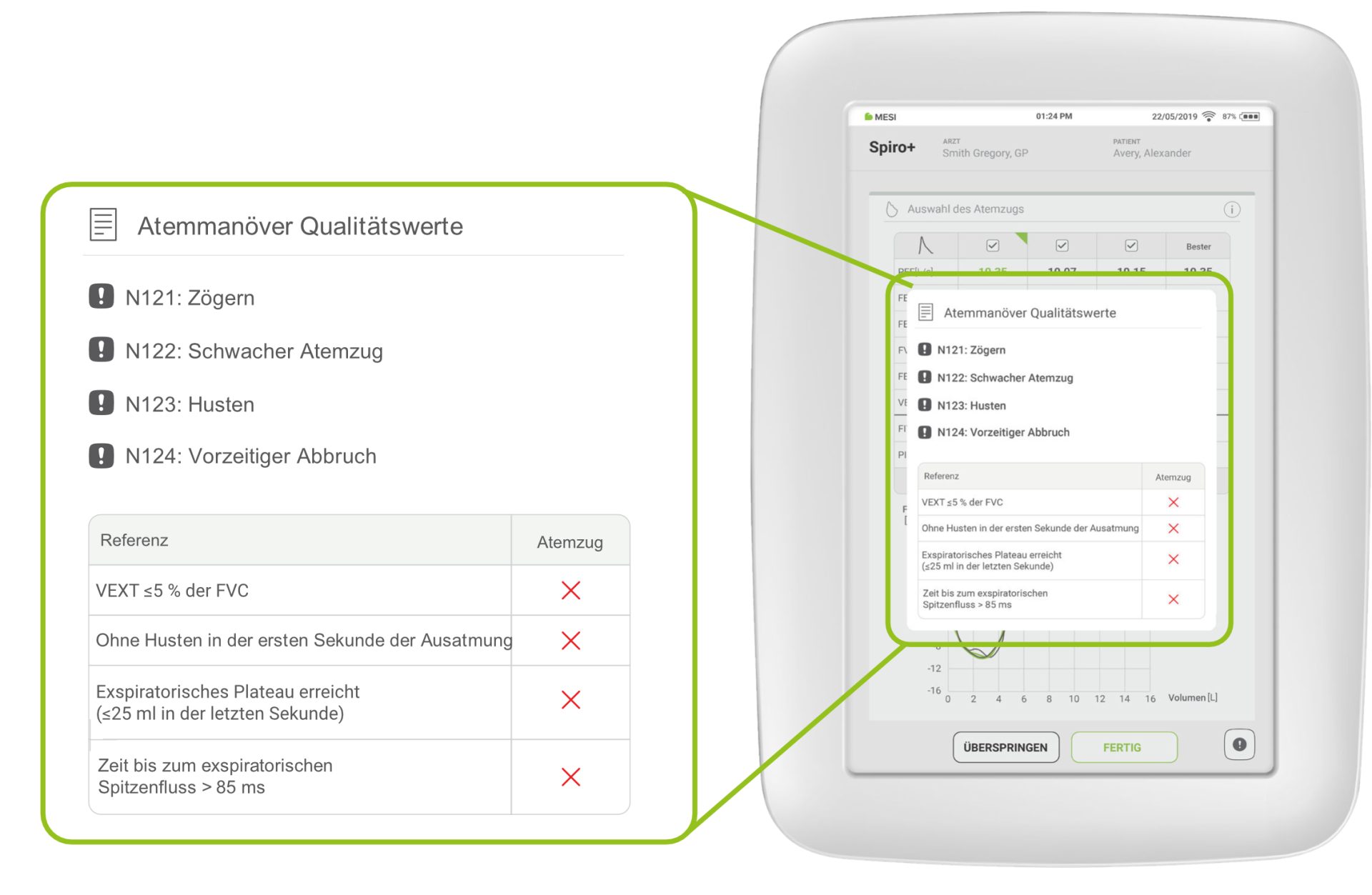
Hier ist ein Beispiel, wenn keines der Akzeptanzkriterien erfüllt ist:
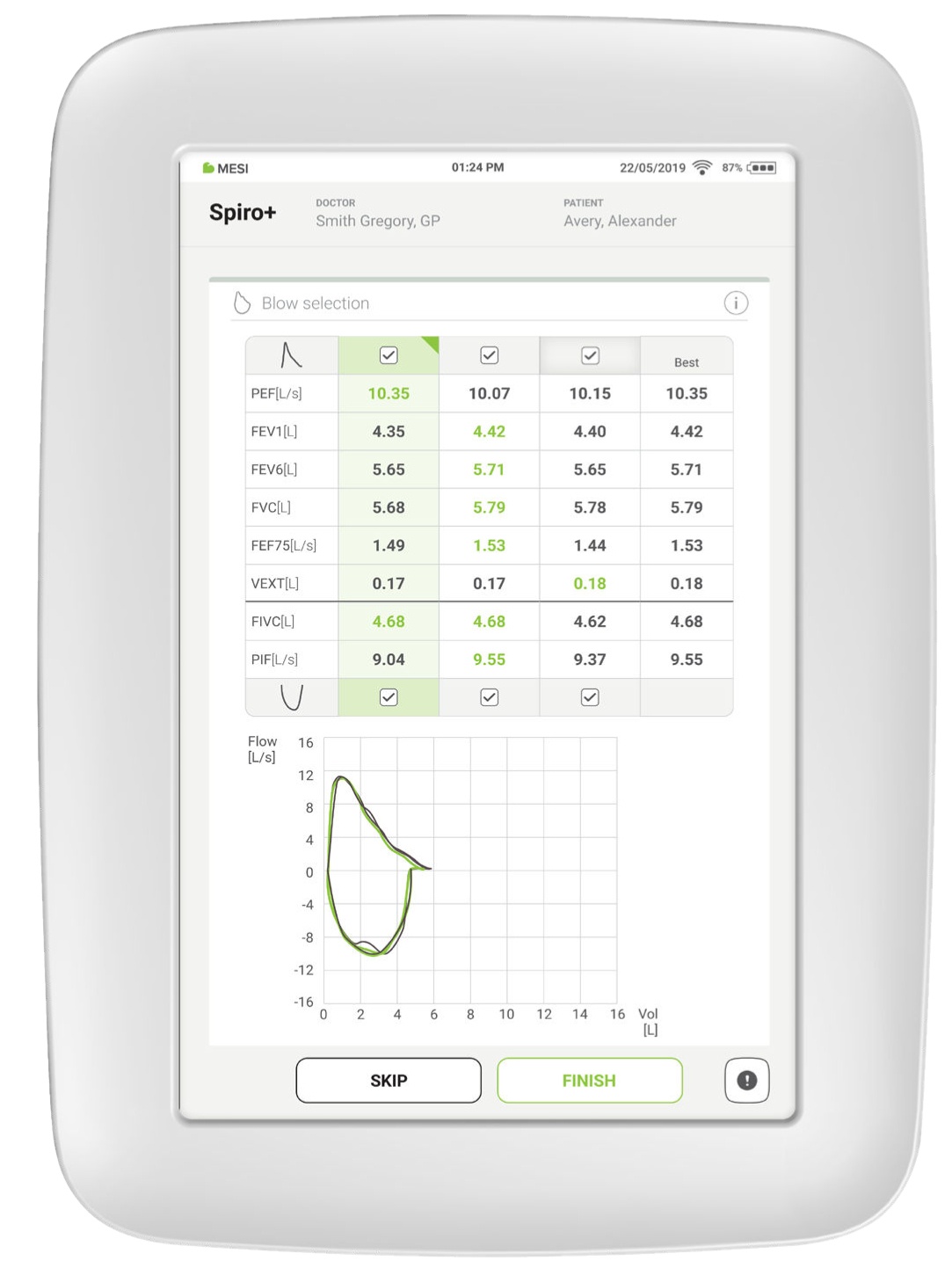
Auswahl der besten Ergebnisse (BestBreath™)
Das Gerät analysiert die Ausatmung und wählt automatisch die beste Kurve aus. Dies ist von Vorteil, wenn zwei Kurven sehr ähnlich waren. Es besteht jedoch auch die Möglichkeit, alle ausgewählten Manöver abzuwählen und das bevorzugte manuell auszuwählen.
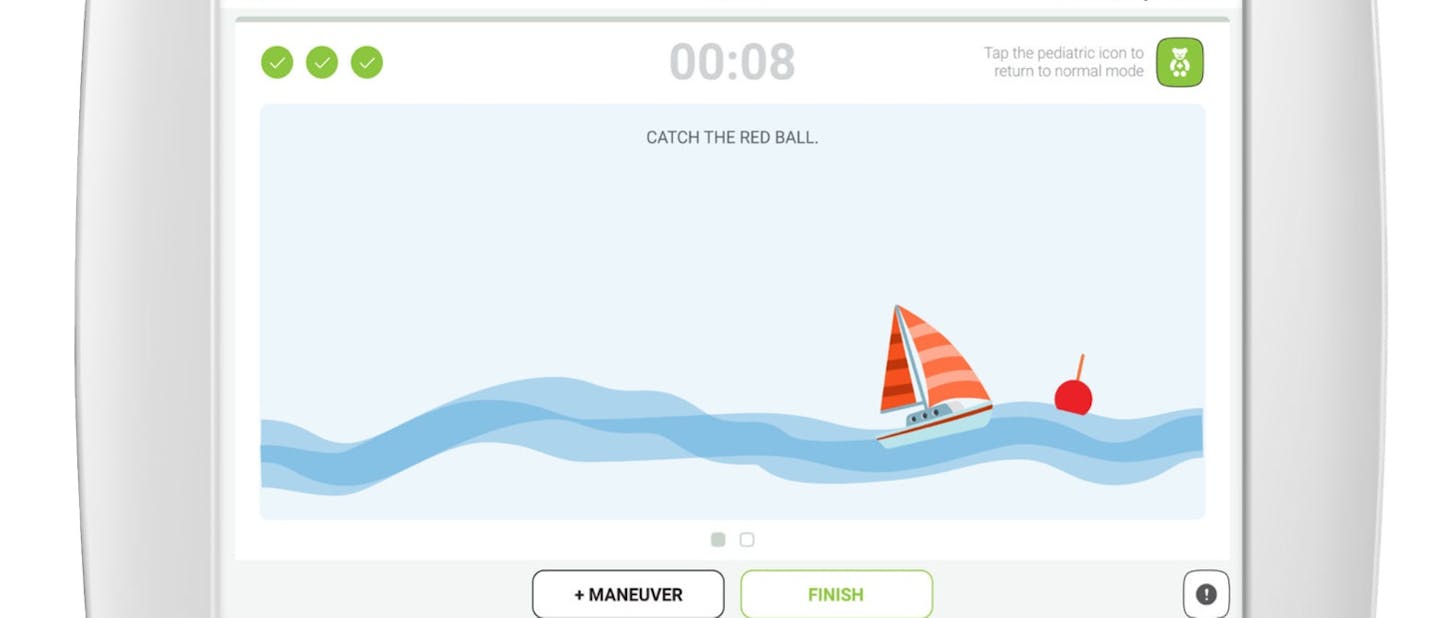
Animationsmodus
Der Animationsmodus wird bei Kindern verwendet. Er wurde entwickelt, um die psychologischen Eigenschaften von Kindern zu berücksichtigen, während sie durch den Spirometrie-Test geführt werden. Während der Patient pustet, nähert sich das Segelboot der roten Boje. Ein Atemstoß ist erfolgreich beendet, sobald das Segelboot die Boje berührt und das grüne Häkchen erscheint.
Im MESI mTABLET SPIRO basiert der Animationsmodus auf den ATS/ERS-Kriterien 2019 [16].

Erkrankungen, die mit Spirometrie häufig diagnostiziert werden
Ein vergleich verschiedener Spirometrie-geräte
Lernen Sie, wie eine SPIROMETRIE erfolgreich durchgeführt wird!
 Holen Sie sich jetzt das kostenlose E-Book
Holen Sie sich jetzt das kostenlose E-Book[1] American Lung Association. Spirometry. What Is Spirometry and Why It is Done. Accessed 19.10.2023. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/spirometry
[2] Graham BL et al. Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med.
2019;200(8):e70e88.https://www.atsjournals.org/doi/full/10.1164/rccm.201908-1590ST
[3] Barreiro TJ and Perillo I. An Approach to Interpreting Spirometry. Am Fam Physician. 2004;69(5):1107-1115. https://www.aafp.org/pubs/afp/issues/2004/0301/p1107.html#afp20040301p1107-b1
[4] The McGill Physiology Virtual Lab. Theory. Lung Diseases. Accessed 15.10.2023. https://www.medicine.mcgill.ca/physio/vlab/other_exps/resp/Lungdiseases_n.htm
[5] NDD Medical Technologies. PFT Testing for cardiopulmonary disease. Accessed 14.10.2023. https://nddmed.com/pulmonary-function-testsolutions/pft-testing-in-cardiology
[6] Hirsch, L. Lungs and Respiratory System. Nemours KidsHealth. Accessed 13.10.2023. https://kidshealth.org/en/parents/lungs.html
[7] iebens AA, Heath DA, Beers MF, Elliott DH, Klocke RA, Weibel ER, Burri PH, Cherniack NS. Human Respiratory System. Encyclopedia Britannica.3.7.2023. Accessed 15.11.2023. https://www.britannica.com/science/human-respiratory-system.
[8] Spirometry. (2023, September 26). Wikipedia. https://en.wikipedia.org/wiki/Spirometry
[9] Towards a good asthma diagnosis in adults. Recent guidelines from the ERS. Soundcloud. Accessed 28.5.2023. https://soundcloud.com/erspodcasts/towards-a-good-asthma-diagnosis-in-adults-recent guidelines-from-the-ers?utm_source=channel.ersnet.org&utm_campaign=wtshare&utm_medium=widget&utm_content=https%253A%252F%252Fsoundcloud.com%252Ferspodcasts%252Ftowards-a-goodasthma-diagnosis-in-adults-recent-guidelines-from-the-ers).
[10] Lamb K, Theodore D, Bhutta BS. Spirometry. [Updated 2023 Jul 17]. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.https://www.ncbi.nlm.nih.gov/books/NBK560526/
[11] Moore VC. Spirometry: step by step. Breathe 2012 8: 232-240. Doi: 10.1183/20734735.0021711 https://breathe.ersjournals.com/content/8/3/232
[12] Pulmonary Function Test (PFT) Explained Clearly.
MedCram. Accessed 17.10.2023. https://www.medcram.com/courses/pulmonary-functiontest-pft-explained-clearly
[13] Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Lp MSM, Zheng J, Stocks J and the ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 2012; 40: 1324–1343. Doi: 10.1183/09031936.00080312. https://erj.ersjournals.com/content/40/6/1324
[14] Sylvester KP, Clayton N, Cliff I et al. ARTP statement on pulmonary function testing. 2020. BMJ Open Respiratory Research 2020;7:e000575. Doi: 10.1136/bmjresp-2020-000575. https://bmjopenrespres.bmj.com/content/7/1/e000575
[15] Luostarinen, E. Open circuit spirometry and closed circuit spirometry. 2021. Medikro. Accessed 10.10.2023. https://medikro.zendesk.com/hc/enus/articles/4407904014481-Open-circuit-spirometry-and-closed-circuit-spirometry
[16] Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, Hallstrand TS, Kaminsky DA, McCarthy K, McCormack MC, Oropez CE, Rosenfeld M, Stanojevic S, Swanney MP, Thompson BR. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019 Oct 15;200(8):e70-e88. doi:10.1164/rccm.201908-1590ST. PMID:31613151; PMCID: PMC6794117. https://www.atsjournals.org/doi/epdf/10.1164/rccm.201908-1590ST?role=tab
[17] Mhagami, C. Spirometry – What is normal and abnormal?. 28.7.2022. iOH. Accessed 19-10-2023. https://ioh.org.uk/2022/07/spriromety-what-isnormal-and-abnormal/
[18] Stanojevic S, Wade A, Stocks J. European Respiratory Journal 2010 36: 12-19; Doi: 10.1183/09031936.00143209. https://erj.ersjournals.com/content/36/1/12.long#sec-5
[19] Sim YS, Lee JH, Lee WY, Suh DI, Oh YM, Yoon JS, Lee JH, Cho JH, Kwon CS, Chang JH. Spirometry and Bronchodilator Test. Tuberc Respir Dis (Seoul). 2017 Apr;80(2):105-112. doi:10.4046/trd.2017.80.2.105. Epub 2017 Mar 31. PMID: 28416951; PMCID: PMC5392482. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5392482/
[20] Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. European Respiratory Journal 1993 6: 5-40. Doi:10.1183/09041950.005s1693. https://erj.ersjournals.com/content/6/Suppl_16/5
[21] Flow-Volume Loops. 15.2.2021. MedSchool. Accessed 13.10.2023. https://medschool.co/tests/lung-function/flow-volume-loops
[22] Asthma. 4.5.2023. World Health Organization. Accessed 12.10.2023. https://www.who.int/news-room/fact-sheets/detail/asthma
[23] Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018 Feb 24;391(10122):783-800. doi: 10.1016/S0140-6736(17)33311-1. Epub 2017 Dec 19. PMID: 29273246. https://pubmed.ncbi.nlm.nih.gov/29273246/
[24] What Happens in Your Airways When You Have Asthma? Asthma and Allergy Foundation of America. Accessed 13.9.2023. https://community.aafa.org/blog/what-happens-in-your-airways-when-you-have-asthma
[25] Symptoms. Asthma. NHS. Accessed 14.10.2023. https://www.nhs.uk/conditions/asthma/symptoms/
[26] Causes. Asthma. NHS. Accessed 14.10.2023. https://www.nhs.uk/conditions/asthma/causes/
[27] Peak flow test. NHS. Accessed 15.10.2023. https://www.nhs.uk/conditions/peak-flow-test/
[28] Louis R, Satia I, Ojanguren I et al. European Respiratory Society guidelines for the diagnosis of asthma in adults. Eur Respir J 2022; 60: 2101585. doi: 10.1183/13993003.01585-2021)
[29] Treatment. Asthma. NHS. Accessed 14.10.2023. https://www.nhs.uk/conditions/asthma/treatment/
[30] Gupta N, Malhotra N, Ish P. GOLD 2021 Guidelines for COPD—What’s New and Why. Advances in Respiratory Medicine. 2021; 89(3):344-346. https://doi.org/10.5603/ARM.a2021.0015. https://www.mdpi.com/2543-6031/89/3/344
[31] Sandelowsky H., Weinreich UM, Aarli BB et al. COPD – do the right thing. BMC Fam Pract 22, 244 (2021). https://doi.org/10.1186/s12875-021-01583-w
[32] COPD. Mayo Clinic. Accessed 11.10.2023. https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes/syc-20353679
[33] Davis, CP. COPD Lung Symptoms, Diagnosis, Treatment. 11.5.2020. emedicinehealth. Accessed 30.9.2023. https://www.emedicinehealth.com/slideshow_pictures_copd/article_em.htm
[34] Pocket Guide to COPD Diagnosis, Management, and Prevention. A Guide for Health Care Professionals. 2021 Report. Global Initiative for Chronic Obstructive Lung Disease. /https://goldcopd.org/wp-content/uploads/2020/11/GOLD-2021-POCKET-GUIDE-v1.0-16Nov20_WMV.pdf (Updated GOLD guidelines 2021)
[35] Kim S, Oh J, Kim YI et al. Differences in classification of COPD group using COPD assessment test (CAT) or modified Medical Research Council (mMRC) dyspnea scores: a cross-sectional analyses. BMC Pulm Med 13, 35 (2013). https://doi.org/10.1186/1471-2466-13-35
[36] Bronchodilators – Antimuscarinics (LAMA). RESPe. Accessed 1.10.2023. https://www.respelearning.scot/topic-3-treatment/medication/bronchodilators-antimuscarinics-lama
[37] Steroid inhalers. NHS. Accessed 2.10.2023. https://www.nhs.uk/conditions/steroid-inhalers/
[38] Chronic Bronchitis. Cleveland Clinic. 24.1.2023. Accessed 13.10.2023. https://my.clevelandclinic.org/health/diseases/24645-chronic-bronchitis
[39] Bulgakova K. COPD (chronic obstructive pulmonary disease). Emphysema of the lungs. Lung disease. Infographics. Getty Images/iStockphoto. Uploaded 15.4.2023. ID: 1312420956. Accessed 14.10.2023. https://www.istockphoto.com/vector/copd-emphysema-of-the-lungs-lung-diseaseinfographics-vector-illustration-in-gm1312420956-401232676
[40] Bronchitis. 2.12.2022. NIH. Accessed 14.10.2023. https://www.nhlbi.nih.gov/health/bronchitis
[41] Felson, S. Chronic Bronchitis Overview. 13.9.2022. WebMD. Accessed 13.10.2023. https://www.webmd.com/lung/copd/copd-chronic-bronchitis
[42] Bronchitis. Reviewed 23.9.2022. Cleveland Clinic. Accessed 12.10.2023. https://my.clevelandclinic.org/health/diseases/3993-bronchitis
[43] Acute Bronchitis. Johns Hopkins Medicine. Accessed 9.10.2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/acutebronchitis
[44] Alveoli. NCI Dictionary of Cancer Terms. NIH. Accessed 1.10.2023. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/alveoli
[45] Emphysema vs. chronic bronchitis. Reviewed by Biggers A, 1.7.2019. MedicalNewsToday. Accessed 1.10.2023. https://www.medicalnewstoday.com/articles/325616#symptoms
[46] Stang D. and Case-Lo C. COPD and Cough: How They’re Related and What You Should Know. Updated 10.3.2023. healthline. Accessed 13.10.2023. https://www.healthline.com/health/copd/coughing
[47] Emphysema. Cleveland Clinic. Reviewed 29.11.2023. Accessed 12.10.2023. https://my.clevelandclinic.org/health/diseases/9370-emphysema
[48] Pulmonology. Emphysema. UCSF Health. Accessed 29.9.2023. https://www.ucsfhealth.org/conditions/emphysema/treatment
[49] Cystic fibrosis. Medline Plus. NIH. National Library of Medicine. Accessed 30.9.2023. https://medlineplus.gov/genetics/condition/cysticfibrosis/#frequency
[50] Cystic Fibrosis. Reviewed 9.5.2022. CDC. Accessed 25.9.2023. https://www.cdc.gov/genomics/disease/cystic_fibrosis.htm
[51] Cystic fibrosis. Updated 18.10.2023. NHSinform. Accessed 13.9.2023. https://www.nhsinform.scot/illnesses-and-conditions/lungs-and-airways/cystic-fibrosis/
[52] Bronchiectasis. Symptoms of bronchiectasis. Updated 15.6.2023. NHSinform. Accessed 13.9.2023. https://www.nhsinform.scot/illnesses-andconditions/lungs-and-airways/bronchiectasis#symptoms-of-bronchiectasis
[53] Bronchiectasis. Causes of bronchiectasis. Updated 15.6.2023. NHSinform. Accessed 13.9.2023. https://www.nhsinform.scot/illnesses-andconditions/lungs-and-airways/bronchiectasis#causes-of-bronchiectasis
[54] Bronchiectasis. Diagnosing bronchiectasis. Updated 15.6.2023. NHSinform. Accessed 13.9.2023. https://www.nhsinform.scot/illnesses-andconditions/lungs-and-airways/bronchiectasis#diagnosing-bronchiectasis
[55] Bronchiectasis. Treating bronchiectasis. Updated 15.6.2023. NHSinform. Accessed 13.9.2023. https://www.nhsinform.scot/illnesses-andconditions/lungs-and-airways/bronchiectasis#treating-bronchiectasis
[56] Obstructive vs. Restrictive. [image] Pinterest. Accessed 30.9.2023. https://www.pinterest.ph/pin/740982944917386962/
[57] Pneumonitis. 9.3.2018. Mayo Clinic. Accessed 15.10.2023. https://www.mayoclinic.org/diseases-conditions/pneumonitis/symptoms-causes/syc-20352623
[58] Colyer A. Pneumonitis: What you need to know. 18.9.2017. Medical News Today. Accessed 15.10.2023. https://www.medicalnewstoday.com/articles/319451#causes
[59] Pulmonary Fibrosis. Reviewed 4.5.2021. Cleveland Clinic. Accessed 12.10.2023. https://my.clevelandclinic.org/health/diseases/10959-pulmonaryfibrosis
[60] Living with Pulmonary Fibrosis. FAQ. Updated 17.11.2022. American Lung Association. Accessed 14.10.2023. https://www.lung.org/lung-healthdiseases/lung-disease-lookup/pulmonary-fibrosis/patients/living-well-with-pulmonary-fibrosis/living-with-pulmonary
[61] Pulmonary fibrosis. 6.3.2018. Mayo Clinic. Accessed 12.10.2023. https://www.mayoclinic.org/diseases-conditions/pulmonary-fibrosis/symptomscauses/syc-20353690
[62] About pulmonary fibrosis. Causes. Pulmonary Fibrosis Foundation. Accessed 11.10.2023. https://www.pulmonaryfibrosis.org/understanding-pff/about-pulmonary-fibrosis/causes
[63] Sève P, Pacheco Y, Durupt F, Jamilloux Y, Gerfaud-Valentin M, Isaac S, Boussel L, Calender A, Androdias G, Valeyre D, El Jammal T. Sarcoidosis: A Clinical Overview from Symptoms to Diagnosis. Cells. 2021 Mar 31;10(4):766. doi: 10.3390/cells10040766. PMID: 33807303; PMCID: PMC8066110 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066110/
[64] Sarcoidosis. 30.1.2019. Mayo Clinic. Accessed 11.10.2023. https://www.mayoclinic.org/diseases-conditions/sarcoidosis/symptoms-causes/syc-20350358
[65] Sarcoidosis. Reviewed 6.10.2022. NHS. Accessed 16.10.2023. https://www.nhs.uk/conditions/sarcoidosis/
[66] Stanojevic S, Kaminsky DA, Miller MR, Thompson B, Aliverti A, Barjaktarevic I, Cooper BG, Culver B, Derom E, Hall GL, Hallstrand TS, Leuppi JD, MacIntyre N, McCormack M, Rosenfeld M, Swenson ER. ERS/ATS technical standard on interpretive strategies for routine lung function tests. European Respiratory Journal Jul 2022, 60 (1) 2101499; DOI: 10.1183/13993003.01499-2021
[67] [Photo] Shutterstock, cited in: Woodyatt, A. Asthma patients could slash their carbon footprint by switching to ‘greener’ inhalers. 30.10.2023. CNN health. Accessed 7.11.2023.
[68] Ernest Z. What are the structure and function of alveoli? [image] Socratic Q&A. Anatomy & Physiology. 15.6.2016. Accessed 13.11.2023. https://socratic.org/questions/what-are-structure-and-function-of-alveoli